Critical Access Hospitals
A Critical Access Hospital (or “CAH”) is a particular type of rural hospital (or one grandfathered in as rural) that is designated as such by the Centers for Medicare and Medicaid Services (CMS). For more information on CAH designation, payments, grants and resources, here is a Critical Access Hospital Fact Sheet.
- State Operations Manual: Chapter 2— The Certification Process: This document from the Centers for Medicare and Medicaid Services (CMS) reviews the requirements for initial certification as well as guidance for relocating CAHs.
- Appendix W of the State Operations Manual: Survey Protocol, Regulations and Interpretive Guidelines for Critical Access Hospitals (CAHs) and Swing-Beds in CAHs
- CMS Transmittals: CMS communications on new or changed policies and procedures.
- A “Swing Bed” is a hospital room that can switch from acute care status to skilled care status. Here is a fact sheet about swing beds.
Location and Distance Regulations:
The federal guidance for the Flex Program requires states to undertake programs and activities that support Quality Improvement (QI) activities of Critical Access Hospitals (CAHs). The Wisconsin Flex Program assists CAHs with various aspects of quality improvement activities, including program planning, data submission, data management and analysis, and best practice development. And, the Wisconsin Flex Program works with the following partners and uses these additional resources to assist CAHs with quality improvement activities.
Organizations and Partners in Quality
Statewide:
- Wisconsin Hospital Association (WHA)
- Metastar – Wisconsin’s quality improvement organization (QIO) that works with health care providers to improvement quality of care.
- Rural Wisconsin Health Cooperative – Offering quality improvement services and programs geared to WI’s rural hospitals and CAHs.
- Wisconsin Collaborative for Healthcare Quality (WCHQ)
Nationwide:
- National Rural Health Resource Center – Resources, tools, and webinars focusing on rural hospital and Critical Access Hospital quality improvement.
- American Heart Association
- National Rural Health Association
Quality Improvement Resources
- Centers for Medicare and Medicaid Services (CMS) – Rules, regulations, tools, resources, and policy briefings directly related to Medicare, Medicaid, and their impacts on CAHs.
- Hospital Compare – CMS’ public quality measures data reporting tool.
- QualityNet – Established by CMS and includes health care quality improvement research, news, data reporting tools, and other information used for health care quality improvement.
- Joint Commission – Includes quality improvement certification, standards, and measurement criteria for hospitals, including CAHs.
- Flex Monitoring Team – This website includes CAH specific quality and patient safety data, reports and studies.
- Agency for Healthcare Research and Quality (AHRQ) – Provides tools and research aimed at quality improvement and patient safety, health care coverage expansion, and addressing the Triple Aim.
MBQIP is a federal quality improvement initiative utilizing measures deemed relevant to rural settings. In Wisconsin, the project is managed by the Wisconsin Office of Rural Health. Rural hospitals report measures in the areas of HCAHPS, Emergency Department Transfer Communications (EDTC), outpatient, and influenza immunization. More detailed information and resources are below, and feel free to contact Kathryn Miller at 608‑261‑1891 with questions.
The Wisconsin Office of Rural Health’s Flex Program has consistently received national recognition for MBQIP performance. In 2017, the Health Resources and Services Administration announced that Wisconsin Critical Access Hospitals had the highest reporting rates and levels of improvement nationally; Since 2019, Wisconsin CAHs have been among the top ten.
The links below provide more information.
Overview
Patient Safety
Outpatient
EDTC
HCAHPS
All hospitals, regardless of size and organizational structure, benefit from analyzing financial and operational performance. The Wisconsin Flex Program identifies financial and operational strengths and challenges in CAHs to implement activities designed to increase profitability.
Performance Improvement Resources and Links
- American Hospital Association – Performance improvement policy briefings, reports, and resources.
- County Health Rankings (CHR) – Measures vital health factors and outcomes in every state on a county-by-county level, and provides a useful way to explore the size and nature of health disparities in Wisconsin. It also emphasizes how state and community leaders can take action to create healthier communities.
- Flex Monitoring Team – Performance improvement data, research and policy briefings related to Critical Access Hospitals.
- National Rural Health Resource Center – Resources, tools, and webinars focusing on rural hospital and Critical Access Hospital performance improvement.
- Financial Data Reports on Wisconsin’s Critical Access Hospitals
- Rural Health Information Hub (RHIhub) (formerly the Rural Assistance Center, or RAC) – A rural and social services online library that focuses on funding opportunities, tools, resources, studied and other publications, events, and news.
- Wipfli LLP – Educational events for CAHs.
Billing and Coding Regulations:
- Medicare Billing Information for Rural Providers and Suppliers
- ICD 10 Regulations and Information – Rules, regulations, and the latest news on ICD-10
- Info onICD 11
The SHIP program—Small Rural Hospital Improvement Program—is a federal grant program of the Health Services and Resources Administration (HRSA), and is administered in Wisconsin by the Wisconsin Office of Rural Health. All Critical Access Hospitals and small rural hospitals with fewer than fifty beds are eligible for the program.
What Can SHIP Funds Be Used For?
There are two ways to take part in the SHIP program:
Option 1) A SHIP-Eligible Project
Under this option, you choose a project to purchase from a menu of eligible services.
What kinds of projects can SHIP fund?
SHIP projects can fund three main categories: value-based purchasing, Accountable Care Organization, and Payment Bundling/PPS. Federal guidelines state that hospitals that receive SHIP funds must use those funds to purchase training or hardware and software for the following valid areas:
- Quality Reporting data collection—like payment for a core measures vendor,
- HCAHPS vendor fees,
- Billing coding systems,
- Telemedicine purchases,
- Training registrations.
The following are not eligible:
- Equipment outside of telemedicine purchases,
- Staff time and fringe, including time spent at trainings,
- Travel costs,
- Food and beverages.
If you choose this option, your hospital is required to comply with University of Wisconsin-Madison Purchasing rules.
The National Rural Health Resource Center has created a SHIP Allowable Investments Search Tool that you can consult to confirm if an expense may be reimbursed using SHIP grant funds.
Option 2) Dashboard Project
Under this option, you participate in our Dashboard Project, administered in collaboration with the Wisconsin Hospital Association Information Center (WHAIC).
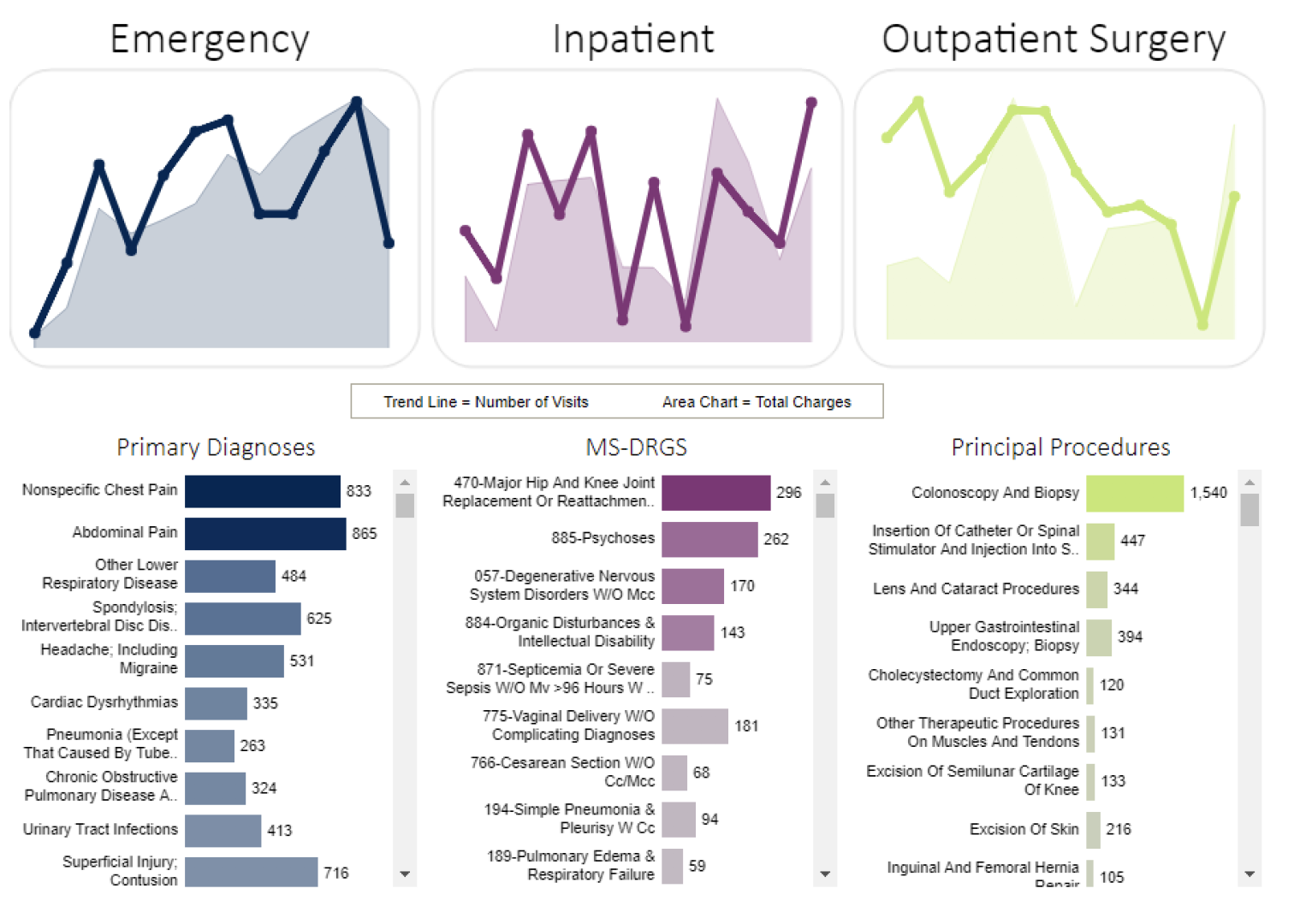
What is the Dashboard?
The dashboard tool provides financial, quality, and other data/information for rural hospitals. The web-based tool is completely interactive, so you can customize it to meet your needs. The tool supports the comparison of rural hospital(s) to each other and/or to a rural cohort.
What does the Dashboard let me do?
- Examine hospital and Ambulatory Surgery Center resources and services
- Analyze patient populations
- Identify patterns, relationships, anomalies, and trends in services, patient populations and other factors
- Evaluate charges and utilization for a specific service, hospital, ASV or market segment
- Explore market opportunities and patterns for key services
- Study payer mix impacts on charges, services and patient populations
- Analyze quality metrics and financial data
What are the current dashboards?
- Hospital summary
- Top visit categories
- Market share
- Top CPT codes
- Place of service
- Financial charts
- Shared patients
- Service lines
- Quality indicators
- Readmissions
- ED returns
For more on the Rural Health Dashboard Project, view a brochure from the Wisconsin Hospital Association Information Center.
The Application
The Wisconsin Office of Rural Health lets the hospitals who are eligible for SHIP know how and when to apply. WORH is affiliated with the University of Wisconsin-Madison School of Medicine and Public Health—so they are involved when it comes to contracts, billing, and invoicing.
Applications are submitted electronically. You must complete the online SHIP application, no matter which option you choose. A link to the application will be posted here when it becomes available.
You will be required to report on the progress of your current SHIP project, so you will need to know who is overseeing your hospital’s SHIP grant. Two “signatures” are required, one from the CEO and one from the SHIP Project Director. Electronic, typed signatures are acceptable.
Deadlines/Timeline
The SHIP grant is from June 1-May 31 every year. SHIP applications typically become become available in December, and are due to our office in January. Exact timing will depend on when the federal office (HRSA) releases the SHIP grant application. (Hospitals may not spend money before the contract is signed and counter-signed.)
Below is a timeline of SHIP deadlines, but the dates are subject to change. More updates are sent out to our listserv; if you would like to be added to the list that contains important updates, contact Megan Polster, Program Assistant, at mepolster@wisc.edu or (608) 261-1891.
May 31. SHIP grant year ends. Last date a purchase may be made for reimbursement.
June 1. SHIP grant year begins.
June. WORH will notify hospitals of the exact amount of funding for the new SHIP year.
June 15. Final deadline to submit invoices for reimbursement for the passed SHIP year.
June/July. UW-Purchasing sends contracts to hospitals. Once completed, hospitals may make purchases and invoice WORH for reimbursement.
August-May 31. After the UW-Madison Purchasing contract is signed and countersigned, hospitals may begin to send invoices to WORH for reimbursement as purchases are made.
December. Application for the next SHIP year distributed to hospitals. All hospitals that wish to receive SHIP funds must complete an application.
Invoicing Instructions

Complete the invoicing template.
Download the SHIP Template.
Here is an Example SHIP Invoice.
The Purchase Order number and the total SHIP grant award can be found on your Funding Award agreement. Both of those numbers will change each year, so make sure you have your current year agreement.
Attach a copy of the original invoice from your vendor. Don’t forget to sign the invoice.
Send to the Wisconsin Office of Rural Health.
Invoices (and questions about invoices) can be directed to Megan Polster, Program Assistant, at mepolster@wisc.edu or (608) 261-1891.
Some tips: The award dollar amount will always be specific and never matches your invoices—but that’s okay. Let’s say you have an invoice from Press Ganey for $12,000 for HCAHPs surveys, and the SHIP award is $11,673. No problem. Report the expense date, description and amount on the template, then enter the amount of the SHIP award ($11,673) in the TOTAL DUE box.
Questions?
Contact Megan Polster, Program Assistant, at mepolster@wisc.edu or (608) 261-1891.
The Wisconsin Office of Rural Health receives grant funding from the Federal Office of Rural Health Policy (FORHP) for the Medicare Rural Hospital Flexibility (Flex) Program. The Flex Program, established by Congress in 1997, assisted small hospitals in converting to a Critical Access Hospitals (CAH) designation – decreasing rural hospital closures and improving rural health care access. The Flex Program has evolved over recent years, and now assists CAHs with quality improvement, financial and operational improvement, population health, and integration of Emergency Medical Services (EMS).
The Wisconsin Office of Rural Health’s Flex Program has received national recognition for Medicare Beneficiary Quality Improvement Project (MBQIP) performance. The Health Resources and Services Administration announced that Wisconsin Critical Access Hospitals have some of the highest reporting rates and levels of improvement nationally over the past several years.
AdventHealth Durand – Durand
Amery Regional Medical Center – Amery
Ascension Calumet Hospital– Chilton
Aspirus Stanley Hospital – Stanley
Aspirus Tomahawk Hospital – Tomahawk
Aspirus Eagle River Hospital – Eagle River
Aspirus Landglade Hospital – Antigo
Aspirus Medford Hospital & Clinics – Medford
Aspirus Merrill Hospital – Merrill
Bellin Health Hospital and Clinic – Oconto
Black River Memorial Hospital – Black River Falls
Burnett Medical Center – Grantsburg
Crossing Rivers Health Medical Center – Prairie du Chien
Cumberland Memorial Hospital – Cumberland
Door County Medical Center – Sturgeon Bay
Edgerton Hospital and Health Services – Edgerton
Essentia Health St. Mary’s Hospital – Superior – Superior
Grant Regional Health Center – Lancaster
Gundersen Boscobel Area Hospital & Clinics – Boscobel
Gundersen Tri-County Hospital & Clinics – Whitehall
Gundersen Moundview Hospital & Clinics – Friendship
Gundersen St. Joseph’s Hospitals & Clinics – Hillsboro
HSHS St. Clare Memorial Hospital – Oconto Falls
Hayward Area Memorial Hospital – Hayward
Hudson Hospital and Clinics – Hudson
Indianhead Medical Center – Shell Lake
Marshfield Medical Center- Ladysmith – Ladysmith
Marshfield Medical Center- Neillsville – Neillsville
Marshfield Medical Center- Park Falls – Park Falls
Mayo Clinic Health System Bloomer – Bloomer
Mayo Clinic Health System Franciscan Healthcare – Sparta
Mayo Clinic Health System Barron – Barron
Mayo Clinic Health System Menomonie – Menomonie
Mayo Clinic Health System Osseo – Osseo
Memorial Hospital of Lafayette County – Darlington
Memorial Medical Center – Ashland
Mercy Walworth Hospital and Medical Center – Lake Geneva
Osceola Medical Center – Osceola
Prairie Ridge Health – Columbus
Reedsburg Area Medical Center – Reedsburg
Richland Hospital, Inc. – Richland Center
River Falls Area Hospital – River Falls
SSM Health Ripon Community Hospital – Ripon
SSM Health Waupun Memorial Hospital – Waupun
Southwest Health Center – Platteville
Spooner Health System – Spooner
St. Croix Regional Medical Center – St. Croix Falls
Stoughton Health – Stoughton
ThedaCare Medical Center – Berlin
ThedaCare Medical Center – New London
ThedaCare Medical Center – Shawano
ThedaCare Medical Center – Waupaca
ThedaCare Medical Center – Wild Rose
Tomah Health – Tomah
Upland Hills Health – Dodgeville
Vernon Memorial Healthcare – Viroqua
Western Wisconsin Health – Baldwin
Westfields Hospital – New Richmond
2023 Pediatric Respiratory Care 3-part Series
Webinar 1: Pediatric Respiratory Care: Updates and Evidence Based Practices. February 8, 2023, with Dr. Allie Hurst, Pediatric Emergency Medicine, UW School of Medicine and Public Health.
Webinar 2: Non-Accidental Trauma: Recognizing and Reporting Child Abuse in the Emergency Department. March 7, 2023. 12 PM – 1 PM CT
MP4 file can be found on our YouTube Channel.
Webinar 3: Pediatric Fever of Unknown Origin.
March 16, 2023. 12PM – 1PM.
MP4 File can be found on our YouTube Channel.
2023 CAH Finance Webinar 3-part Series
CAH Financial and Operational Best Practices
In an environment of increasing cost and stagnant reimbursement, CAHs must do everything necessary to improve their financial stability. This presentation identifies a small but focused set of tactics CAHs can implement to improve their financial and operational performance.
WI #1 – CAH Financial & Operational Best Practices_Presentation Slides
CAH Reimbursement: Using the Cost Report to Reveal Opportunities
Most organizations view the Medicare Cost Report as a tedious administrative task and to many CFOs, a hassle. As a result, CAHs often fail to acknowledge the direct impact the cost report has on CAH reimbursement. This presentation highlights the importance of the Medicare Cost Report and explains how to leverage the cost report as a part of the managerial decision-making process.
WI #2 – CAH Cost Report – Presentation Slides
Establishing a High-Functioning Revenue Cycle Department
Revenue cycle remains one of the best opportunities for hospitals to improve operational efficiencies due to its complexity and core function. This presentation walks participants through the full revenue cycle value chain while identifying common pitfalls that impact revenue.
WI #3 – Maintaining a High Functioning Revenue Cycle Department – Presentation Slides
For more information on the series, please contact Megan Polster.